Using mHealth to improve eye care in remote areas of Iran
Related content
Primary health workers are using a new digital mHealth tool to support eye health screening and management in Iran.
Mobile communication technology in health (mHealth) offers opportunities to improve prevention and care for non-communicable diseases (NCDs).1 Most evidence comes from high-income countries;2 however, recent studies show that this technology is also effective at community level in low- and middle-income countries (LMICs).3,4 It is possible to enhance health care through mobile technology, both on- and offline, in different settings.5
In Iran there is one ophthalmologist and one optometrist per 40,000 and 45,000 people, respectively. Although this meets the World Health Organization’s recommendations, the distribution in the country is uneven.6 Recent population-based studies showed that the proportion of avoidable eye disorders is high even in areas with available human resources and infrastructure due to inadequate prevention.7,8
mHealth, also known as telemedicine, may facilitate cost-effective use of available resources and decrease unnecessary workload on referral centres. To enable early detection and better management and monitoring of vision-threatening conditions, provide timely follow-up and prevent ocular morbidity, we designed a community-based mHealth screening, management and monitoring tool to be integrated into the national health care system. With this tool, primary health care (PHC) workers – the community health providers known as Behvarz in Iran – have the opportunity to screen the population in remote areas, upload data and digitally consult with an ophthalmologist in an urban referral centre.
How does it work?
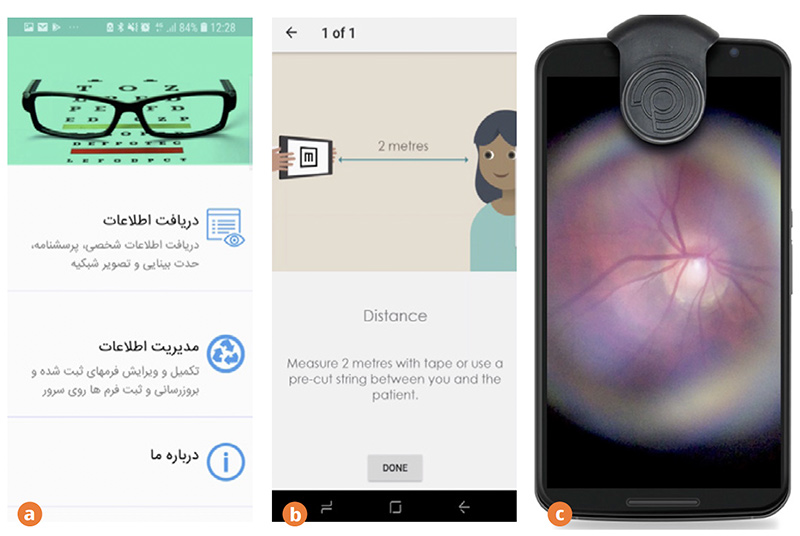
The tool has two components: a mobile application and web-based software. The mobile application consists of digital survey forms, an integrated software application (Peek Acuity) for obtaining visual acuity (VA),10 integrated hardware for optimizing retinal imaging (Peek Retina),11 and a management system for the PHC workers.
The forms and screening tests were developed based on focus group discussions with professionals and health providers.9
There are four steps:
- The PHC workers use the mobile application to enter each patient’s demographic and eye health history data, visual acuity and retinal images.
- The information is uploaded to the customised web-based system.
- An ophthalmologist in a reading centre reviews the information on the web-based system and provides a management plan.
- Participants receive their results and follow-up advice, if needed, using an automated SMS (text message) system.
Testing the mHealth tool
An intervention trial on community members was carried out to test the effectiveness and acceptability of the tool. A representative sample of 50+ residents from 27 enumeration areas were enrolled through door-todoor visits of the households with a random and compact segment sampling method. Ethical approval was granted by Shahid Behesthi University of Medical Sciences in Tehran.
The study had three arms:
- mHealth intervention: using mobile application for data collection and screening tests.
- Conventional intervention: using paper-based forms, Snellen chart for measuring VA and fundus photography equipment for fundus imaging.
- Control arm: using paper-based forms, no further intervention.
Participants with presenting VA≤20/40 in either eye were referred to an ophthalmologist for further evaluation. An ophthalmic assistant conducted retinal imaging, using Peek Retina, at the local PHC units. Retina specialists in a central reading centre reviewed retinal images and, if necessary, made further referral plans.

Results
Over 3,000 residents were enrolled, with 92.1% in the control, 78.4% in the mHealth and 57.7% in the conventional group agreeing to participate..
Of 1,508 participants in vision screening (mHealth =873), (conventional = 635), 608 (40.3%, 95%CI: 37.8-42.8) had ≤20/40 vision in at least one eye and were therefore referred for evaluation (referral rate 35.9% in conventional vs. 43.5% in the mHealth arm, not significant after adjusting for age and need for eye care.
Fundus evaluation was performed in 756 participants with >20/40 presenting visual acuity. Of the 756, 45 (0.6%) had poor quality images (20 [0.5%] in conventional and 25 [0.75%] mHealth arms). Of 711 people with fundus evaluation, 173 (24.3%) had abnormal images (79 [19.6%] in conventional and 94 [26.9%] mHealth arms).
Implications
The findings show a high level of eye care need in the study population. PHC workers were able to examine the eye and transmit images for expert assessment using the mHealth tool.
Making a definite diagnosis and grading of disorders were beyond the objectives of the study; nevertheless, in those who were referred based on fundus imaging, the following abnormalities were found: diabetic retinopathy, age-related macular degeneration, glaucoma, high myopia, chorio-retinal scar, myopic fundus with chorio-retinal atrophy, retinal scars and hyper-pigmentation.
Geographic location and socioeconomic status are factors that may inhibit service provision, use and continuity of care. Appropriate mHealth solutions may provide access to specialist consultation services and early interventions. This mHealth eye-care approach delivers health care to populations that have limited access to specialist services and improves the health care where there are only partial services.
Many advantages of this mHealth solution were identified, including improved resource use, early intervention, avoidance of unnecessary transportation, community-based delivery and engagement, combined medical education and research, cost efficiency, improved medical record documentation and an increased coverage of care.
The mHealth tool is being updated following feedback from different users.
Acknowledgement: The authors would like to express their sincere gratitude to the Peek Vision team in the UK for their great contribution to developing the mHealth tool in this project. We also express our sincere gratitude to Ardeshir Montaseri, the CEO, and the IT team at the Asre Danesh Afzar Co. who adopted and managed this mHealth tool.
References
1 Payne HE, Lister C, West JH, Bernhardt JM. Behavioral functionality of mobile apps in health interventions: a systematic review of the literature. JMIR mHealth uHealth 2015 Feb;3(1): e20.
2 Free C, Phillips G, Galli L, Watson L, Felix L, Edwards P, et al. The Effectiveness of Mobile-Health Technology-Based Health Behaviour Change or Disease Management Interventions for Health Care Consumers: A Systematic Review. Cornford T, editor. PLoS Med 2013 Jan;10(1): e1001362.
3 Xavier D, Gupta R, Kamath D, Sigamani A, Devereaux PJ, George N, et al. Community health worker-based intervention for adherence to drugs and lifestyle change after acute coronary syndrome: a multicentre, open, randomised controlled trial. Lancet Diabetes Endocrinol 2016 Mar;4(3): 244–53.
4 Rubinstein A, Miranda JJ, Beratarrechea A, Diez-Canseco F, Kanter R, Gutierrez L, et al. Effectiveness of an mHealth intervention to improve the cardiometabolic profile of people with prehypertension in low-resource urban settings in Latin America: a randomised controlled trial. Lancet Diabetes Endocrinol 2016 Jan;4(1): 52–63.
5 Royston G, Hagar C, Long L-A, McMahon D, Pakenham-Walsh N, Wadhwani N, et al. Mobile health-care information for all: a global challenge. Lancet Glob Heal 2015 Jul;3(7): e356–7.
6 Mohammadi S-F, Lashay M-R, Ashrafi E, Haghdoust A-A, Alinia C, Lashay A-R, et al. Distribution of ophthalmologists and optometrists in Islamic Republic of Iran and their associated factors. East Mediterr Health J 2017 Feb;22(12): 880–6.
7 Rajavi Z, Katibeh M, Ziaei H, Fardesmaeilpour N, Sehat M, Ahmadieh H, et al. Rapid assessment of avoidable blindness in Iran. Ophthalmology 2011 Sep;118(9): 1812–8.
8 Katibeh M, Blanchet K, Akbarian S, Hosseini S, Ahmadieh H, Burton MJ. ‘Planning eye health services in Varamin district, Iran: a cross-sectional study’. BMC Health Serv Res 2015 Apr;15(1): 140.
9 Katibeh M, Kalantarion M, Sabbaghi H, Mousavi B, Schriver M, Nikkhah H, et al. Designing a screening program for prevention of avoidable blindness in Iran through a participatory action approach. J Ophthalmic Vis Res. 2019;14(1):52.
10 Bastawrous A, Rono HK, Livingstone IAT, Weiss HA, Jordan S, Kuper H, Burton MJ. Development and Validation of a Smartphone-Based Visual Acuity Test (Peek Acuity) for Clinical Practice and Community-Based Fieldwork. JAMA Ophthalmol. 2015;133(8):930.
11 Bastawrous A, Giardini ME, Bolster NM, Shah N, Livingstone IA, Weiss HA, et al. Clinical Validation of a Smartphone-Based Adapter for Optic Disc Imaging in Kenya. JAMA Ophthalmol. 2016;134(2):151-158.

